back to health. back to living.
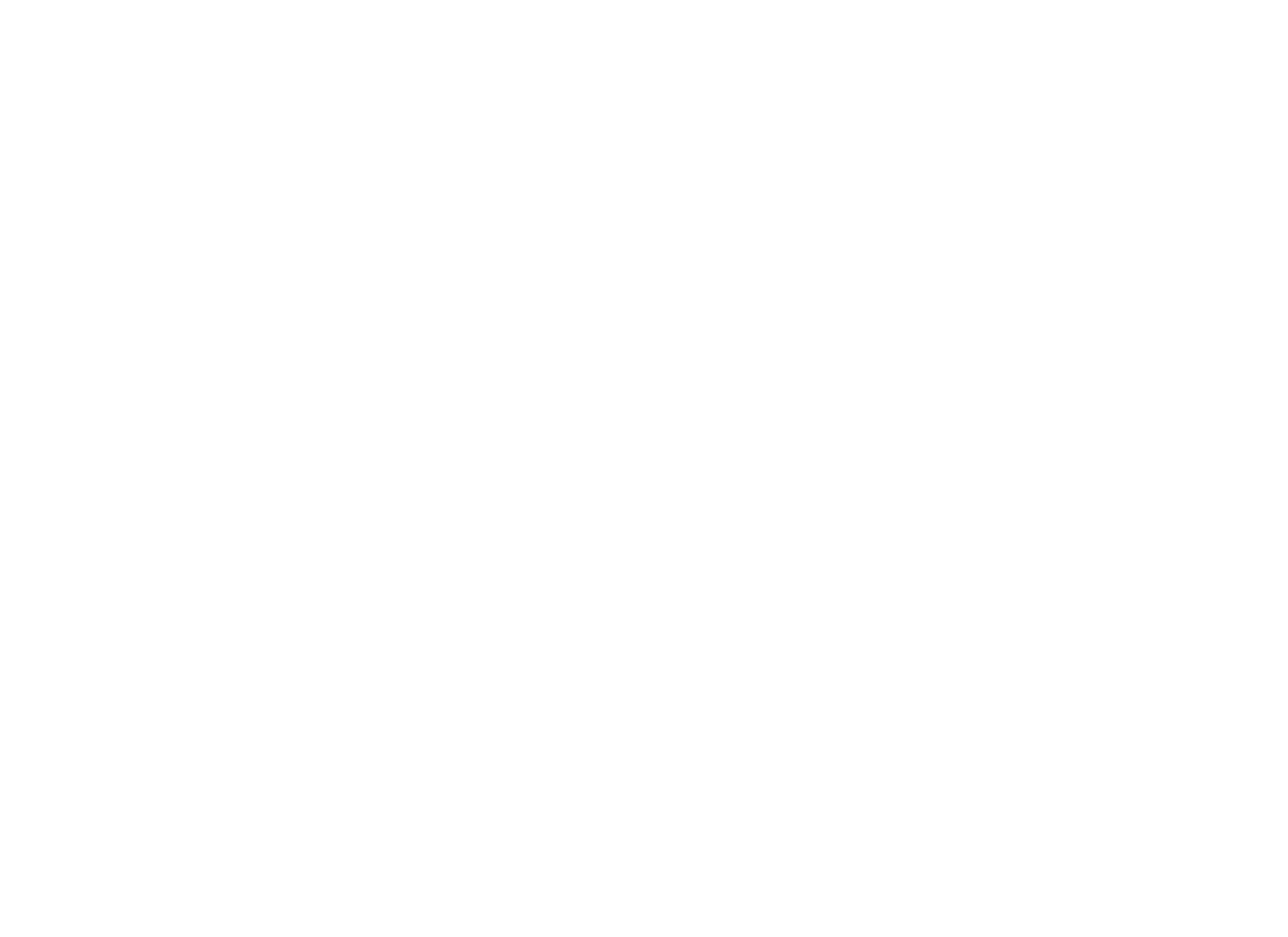
Our state-of-the-art, full-service facility is staffed with caring professionals ready to apply the most advanced medical and surgical technologies to help our patients regain function and live more active and fulfilling lives. We are the leaders in patient-friendly and exceptional Spinal Surgery outcomes in Ventura County.
our services
We restore patients who are suffering
from spinal pain using the safest, least invasive and
most conservative treatment methods possible.
MINIMALLY INVASIVE SPINE SURGERY
This minimally invasive technique is used to remove the herniated portion of a vertebral disc. It is highly effective in eliminating leg pain (sciatica) caused by nerve root compression. The procedure is performed through a small incision on the back.
MINIMALLY INVASIVE SPINE SURGERY
This minimally invasive technique is used to remove the herniated portion of a vertebral disc. It is highly effective in eliminating leg pain (sciatica) caused by nerve root compression. The procedure is performed through a small incision on the back.

ARTIFICIAL DISC REPLACEMENT
This procedure replaces a degenerative or damaged spinal disc with an implant designed to preserve motion in your spine. This procedure is designed to preserve motion in your cervical or lumbar spine.
ARTIFICIAL DISC REPLACEMENT
This procedure replaces a degenerative or damaged spinal disc with an implant designed to preserve motion in your spine. This procedure is designed to preserve motion in your cervical or lumbar spine.

KYPHOPLASTY
This minimally-invasive procedure repairs a vertebral compression fracture. It helps restore the spine’s natural shape. Some patients experience rapid pain relief after the procedure.
KYPHOPLASTY
This minimally-invasive procedure repairs a vertebral compression fracture. It helps restore the spine’s natural shape. Some patients experience rapid pain relief after the procedure.
XLIF®
Unlike traditional back surgery, XLIF® is performed through the patient’s side. By entering this way, major muscles of the back are avoided. This minimally-invasive procedure is generally used to treat leg or back pain caused by degenerative disc disease. It can be performed on an outpatient basis.
XLIF®
Unlike traditional back surgery, XLIF® is performed through the patient’s side. By entering this way, major muscles of the back are avoided. This minimally-invasive procedure is generally used to treat leg or back pain caused by degenerative disc disease. It can be performed on an outpatient basis.

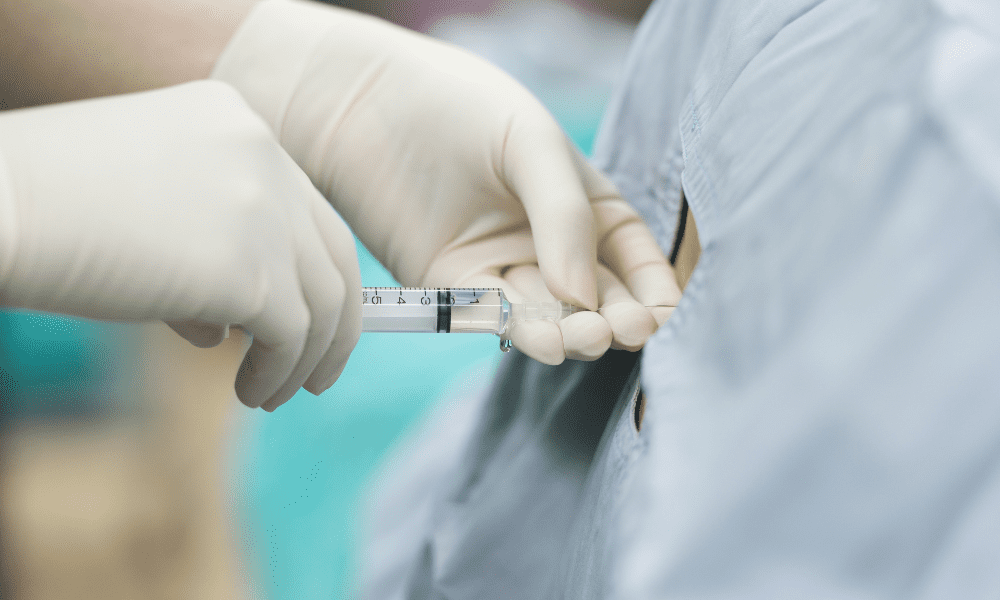
EPIDURAL STEROID INJECTIONS
Cervical Epidural Steroid Injections
These injections relieve pain in the neck, back and extremities caused by pinched nerves in the spine. Conditions such as herniated discs and spinal stenosis can compress nerves, causing inflammation and pain. The medication injected helps decrease the swelling of nerves.
EPIDURAL STEROID INJECTIONS
Cervical Epidural Steroid Injections
These injections relieve pain in the neck, back and extremities caused by pinched nerves in the spine. Conditions such as herniated discs and spinal stenosis can compress nerves, causing inflammation and pain. The medication injected helps decrease the swelling of nerves.
STEM CELL THERAPY
Through regenerative medicine, a person can take advantage of their body’s ability to heal itself by using the healthy stem cells that can be found throughout the body. Laboratory and clinical research has shown that it is possible to use stem cells to restore lost, damaged or aging cells and effectively regenerate tissue in the body.
STEM CELL THERAPY
Through regenerative medicine, a person can take advantage of their body’s ability to heal itself by using the healthy stem cells that can be found throughout the body. Laboratory and clinical research has shown that it is possible to use stem cells to restore lost, damaged or aging cells and effectively regenerate tissue in the body.

WIDE BORE MRI
St Charles Spine Institute, along with St Charles Imaging Center has one of the most advanced diagnostic tools for assisting the physicians to reach confident diagnoses and helping patients feel more comfortable during MR scans.
WIDE BORE MRI
St. Charles Spine Institute, along with St. Charles Imaging Center has one of the most advanced diagnostic tools for assisting the physicians to reach confident diagnoses and helping patients feel more comfortable during MR scans.

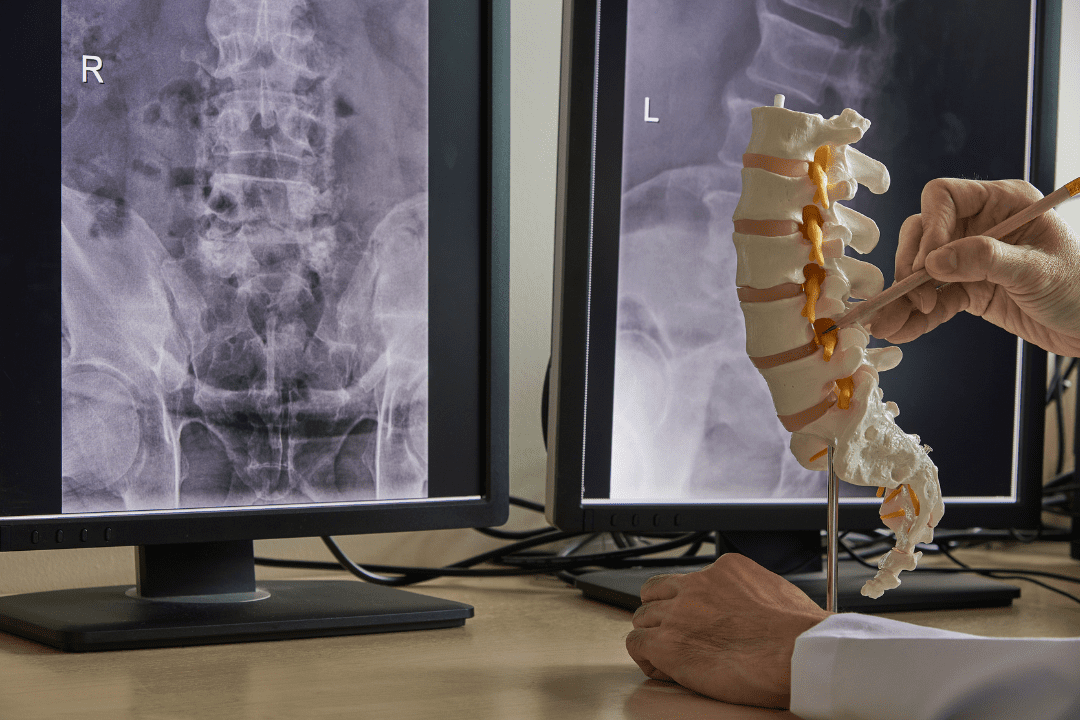
Lumbar Disc Microsurgery
This minimally invasive technique is used to remove the herniated portion of a vertebral disc. It is highly effective in eliminating leg pain (sciatica) caused by nerve root compression. The procedure is performed through a small incision on the back.
Lamina Opened
After creating a small incision directly over the herniated disc, the surgeon creates a small window in the lamina (the bone covering the spinal canal). The pinched nerve root and the herniated disc can be seen through this opening.
Spinal Nerve Moved
The surgeon uses a nerve retractor to gently move the spinal nerve away from the herniated disc.
Herniation Removed
The herniated portion of the disc is removed, eliminating pressure on the nerve root. Only the damaged portion of the disc is removed, leaving any healthy disc material to perform its function as a cushion between the vertebrae.
End of Procedure
The tools are removed, and the spinal nerve returns to its normal position. The incision is closed.
Artificial Cervical Disc Replacement (Mobi-C®)
This procedure replaces a degenerative or damaged spinal disc with an implant designed to preserve motion in your neck. This procedure can relieve the pain of compressed nerves in the cervical spine.
Removing the Disc
In preparation for the procedure, you are positioned on your back. You are anesthetized. The surgeon creates a small incision in the front of your neck. The structures within your neck are gently moved aside to create a path to your spine. The surgeon carefully removes the damaged disc. This leaves a space between the vertebrae.
Inserting the Implant
The implant has three parts: upper and lower metallic plates and a plastic core that sits between them. The plates have teeth designed to hold them securely in place. These teeth are pressed into the upper and lower vertebrae. Over time, bone will grow and attach to these plates.
Motion
Unlike a rigid neck fusion, which locks your neck in a fixed position, the implant is designed to allow you to move your neck more naturally. The components glide smoothly against each other. With the implant, you can turn your head and bend your neck forward, backward and side to side, just as you would with an undamaged disc.
End of Procedure and Aftercare
When the procedure is complete, the incision is closed. You may wear a neck support as you heal. You may benefit from physical therapy. Your surgeon will give you specific instructions to aid your recovery.
Kyphoplasty
This minimally-invasive procedure repairs a vertebral compression fracture. It helps restore the spine’s natural shape. Some patients experience rapid pain relief after the procedure.
Preparation
Before the procedure, you are anesthetized. The physician guides a needle through the skin of your back and into your fractured vertebra. A special x-ray device called a “fluoroscope” helps the physician position the needle.
Balloon Inserted
A balloon device is placed through the needle and into the vertebral body. The physician carefully inflates this balloon to expand the fractured bone. When the balloon is deflated, it leaves a cavity in the middle of the vertebral body. The balloon is removed. For some patients, more than one needle and balloon may be used.
Fracture Stabilized
The physician injects bone cement through the needle. This cement fills the cavity. It hardens inside the vertebral body, stabilizing the fracture.
End of Procedure and Aftercare
When the procedure is complete, the needle is removed. The opening in your skin is closed. Your doctor will give you instructions to aid your recovery.
Lateral Lumbar Interbody Fusion
Unlike traditional back surgery, XLIF® is performed through the patient’s side. By entering this way, major muscles of the back are avoided. This minimally-invasive procedure is generally used to treat leg or back pain caused by degenerative disc disease. It can be performed on an outpatient basis.
Accessing the Spine
The surgeon creates two small incisions in the patient’s side. These incisions are much smaller than those used in traditional back surgery. A probe is inserted through one incision. The second incision is used to help guide the surgical instruments.
Avoiding Nerves
The surgeon uses the probe to stimulate and detect nerves along the side of the spine. When a nerve is found it can be avoided and left undamaged. Fluoroscopic x-ray images also are used to guide the probe to the proper position on the spine.
Dilation Tubes Inserted
A series of dilation tubes are slid over the probe to create a larger opening. Then, a retraction device is used to move aside muscle tissue and gain access to the spine.
Disc Removed
The surgeon operates through the channel created by the retractor. The damaged disc is removed.
Implant Inserted
An implant filled with bone graft is placed into the empty disc space, realigning the vertebral bones. This also lifts pressure from pinched nerve roots. Bone Morphogenetic Protein (BMP) may also be used to encourage bone growth and a strong fusion.
End of Procedure
The morselized bone graft will grow through and around the implant, forming a bone bridge that connects the vertebral bodies above and below. This solid bone bridge is called a fusion.
Cervical Epidural Steroid Injections
This injection relieves pain in the neck, shoulders, and arms caused by a pinched nerve (or nerves) in the cervical spine. Conditions such as herniated discs and spinal stenosis can compress nerves, causing inflammation and pain. The medication injected helps decrease the swelling of nerves.
Lumbar Epidural Steroid Injections
This injection procedure is performed to relieve low back and radiating leg pain. Steroid medication can reduce the swelling and inflammation caused by spinal conditions.
What Are Adult Stem Cells?
Stem cells were discovered over 40 years ago when researchers found that cells derived from bone marrow had the ability to form various tissues. Stem cells are early stage cells that under the right conditions, are capable of developing into other types of cells with the potential to regenerate damaged tissue.
Where Do Adult Stem Cells Come From?
In adults, stem cells are present within variety of tissues and organs, the most common sources being bone marrow and fat (or adipose) tissue. At present, the majority of adult stem cell procedures utilize bone marrow derived stem cells.
Is Stem Cell Therapy Safe, And Does It Work?
Decades of clinical studies have shown that adult stem cells are safe. You should not have any adverse effects following the use of your own stem cells.
What Is The Procedure Like?
A basic stem cell procedure lasts about 45 minutes or less. The physician will retrieve bone marrow percutaneously from the iliac crest of the hip (5 minutes). The aspirated bone marrow will then be concentrated into a smaller volume, devoid of plasma and red blood cells (12 minutes). Finally, the physician will deliver your concentrated stem cells back to the target site for regeneration.
What Is The Recovery Period Like?
After a joint injection, you can typically go back to work. Immediately. It is advised to avoid load-bearing activities for at least 2 weeks. After a disc injection, you should rest for 2-3 days and try to stay off your feet. In any stem cell procedure, anti-inflammatory medications (NSAIDS) should be withheld for 72 hours pre-procedure and one week post-procedure.
How Much Will It Cost?
Currently, insurance companies do not cover stem cell procedures.
How Long Will Stem Cells Last?
The treatment success will depend on your injury, the area that is treated, and your response to the therapy. Ask your doctor if you are a good candidate.
What is Wide Bore MRI?
A Wide Bore MRI is an imaging system that is open to comfortably accommodate all patients (table weight limit is 500lbs). This differs from the traditional tunnel-style magnetic resonance imager in which some patients feel confined and uncomfortable.
How should you prepare for the procedure?
MRI uses a strong magnetic field. Patients will be interviewed prior to the exam and asked if they have any metallic objects in their body. If there is any question of metal fragments being present, you may be asked to have an x-ray that will detect any such objects. In most cases, cardiac stents, artificial heart valves, prosthetic joints, and surgical staples, plates, pins and screws pose no risk during MRI if they have been in place for more than four to six weeks. The REVO Pacemaker by Medtronic is “MRI Conditional.”
Ideal clothing should be worn for your MRI exam; clothing should not have any metal snaps, buttons, or zippers (e.g. sports bra, shorts or pants with elastic waste, jogging suits).
As with all radiological procedures, patients should inform the technologist if there is any chance of pregnancy.
What can a person expect during the MRI study?
The patient is placed on a sliding table by the technologist and positioned comfortably for the study in the bore of the scanner. The technologist leaves the room and programs individual MRI sequences that typically last between 2 and 6 minutes each. A tapping or knocking noise will be heard during the imaging process.
An intercom allows the patient and technologist to communicate with each other at any time during the study. Depending on the number of images necessary, the study will generally take 20-30 minutes. You will be asked not to move during each sequence while breathing normally.
Depending upon the study, a contrast material (gadolinium) may be injected intravenously in an arm vein. This material will enhance certain tissues or blood vessels, making them more conspicuous and aiding diagnosis.